
Sleep apnea and how it is associated with Obesity
Sleep apnea refers to a condition in which
58,988 total views, 111 views today
Home » Migraine and obesity

Sleep apnea refers to a condition in which
58,988 total views, 111 views today

Since the beginning of 20th century, the overall
58,965 total views, 111 views today

New year is the time for new beginnings.
59,665 total views, 111 views today

Weight loss can be tricky business, as it
59,536 total views, 111 views today

According to a recent study, weight loss through
60,435 total views, 111 views today

According to a recent study, preoperative very low
60,436 total views, 111 views today
A recent study conducted on GERD (Gastroesophageal Reflux
60,441 total views, 112 views today
A recent study done to examine the long-term
59,319 total views, 108 views today

Overweight and obesity is a major health concern
29,588 total views, 76 views today

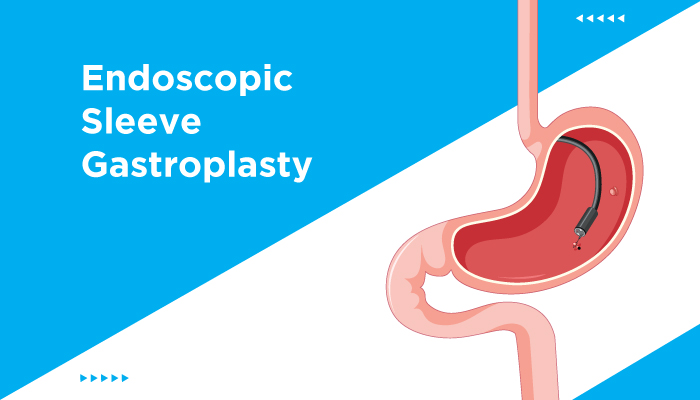
A recent study published in the Journal of
28,777 total views, 75 views today
The findings from a recent study, published in
29,018 total views, 75 views today

The findings of a recent study, published in
29,419 total views, 76 views today