
Sleep apnea and how it is associated with Obesity
Sleep apnea refers to a condition in which
58,996 total views, 119 views today
Home » Time Restricted Eating Improves Metabolic State of Overweight Individuals
A recent study published in the Journal of Clinical Endocrinology and Metabolism indicated that time-restricted eating (TRE), which is a key regimen of intermittent fasting (IF) helps improve metabolic state of overweight individuals.
The study included seventeen randomized controlled trials and involved 899 participants. The study lasted for a span of 4 weeks during which body weight and other metabolic-related parameters were evaluated to find the efficacy of TRE on weight loss.
The results showed that TRE contributed to a significant decrease in body weight and fat mass in overweight participants. However, TRE had no significant effect on other parameters such as waist circumference (WC), blood pressure, glycosylated haemoglobin (HbA1c), and body mass index (BMI). It also had beneficial effects on the lipid spectrum in overweight participants.
Hence, these findings indicate that time-restricted eating is an effective approach to improve the metabolic state of overweight individuals.
Reference:
Source: Liu L, Chen W, Wu D, Hu F. Metabolic Efficacy of Time-Restricted Eating in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Endocrinol Metab. 2022 Oct 3: dgac570.
Source link:

Sleep apnea refers to a condition in which
58,996 total views, 119 views today

Since the beginning of 20th century, the overall
58,972 total views, 118 views today

New year is the time for new beginnings.
59,672 total views, 118 views today

Weight loss can be tricky business, as it
59,543 total views, 118 views today

According to a recent study, weight loss through
60,442 total views, 118 views today

According to a recent study, preoperative very low
60,443 total views, 118 views today
A recent study conducted on GERD (Gastroesophageal Reflux
60,448 total views, 119 views today
A recent study done to examine the long-term
59,326 total views, 115 views today

Overweight and obesity is a major health concern
29,595 total views, 83 views today
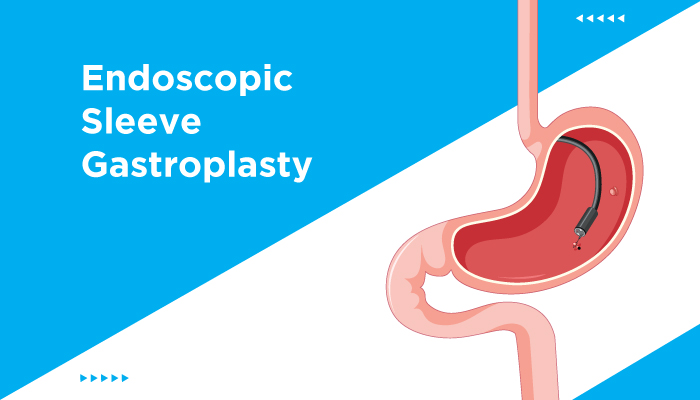
The findings from a recent study, published in
29,025 total views, 82 views today

The findings of a recent study, published in
29,426 total views, 83 views today
Dietary modifications, along with regular exercise, play an
11,943 total views, 25 views today
