
Sleep apnea and how it is associated with Obesity
Sleep apnea refers to a condition in which
58,936 total views, 59 views today
Home » Polycystic Ovarian Syndrome
Polycystic ovary syndrome (PCOS) is a common hormonal condition that affects one in 10 women of reproductive age. Women with PCOS have higher levels of androgens (male hormones that is also present in female), which interrupt normal ovulation and results in irregular periods, acne, excess facial and body hair, and male-pattern baldness. In addition to these characteristic, it increases the risk of infertility and type-2 diabetes.
Though the exact cause of PCOS is unknown, experts believe that a combination of genetic and environmental factors contributes to the condition. Some clinical evidence indicates that there is a close link between obesity and PCOS.
Obesity and PCOS are interlinked and shares a complex connection. According to studies, 40–80% of women with PCOS are reported to be obese. Women with PCOS have insulin resistance, which worsens with obesity and other lifestyle related factors. Being obese, especially in the abdominal region increases the risk of insulin resistance for up to 50%.
Insulin Action in PCOS:Relation with Obesity
Insulin is a peptide hormone produced by beta cells of the pancreas. It plays an important role in controlling blood sugar levels. It control blood glucose by signaling the liver, muscle and fat cells to take in glucose from the blood.
In obese individuals, the cells in muscles, fat, and liver don’t respond well to insulin and fail to take in glucose from the blood. Thus, it result in high blood glucose levels. In order to control blood glucose levels, the pancreas produce large amount of insulin. Excess insulin leads to insulin resistance which in turn decreases the body’s ability to use insulin effectively and thus results in hyperinsulinemia. According studies, about 50–70% of women with PCOS are highly obese and have detectable insulin resistance and hyperinsulinemia [12]. Obesity-associated insulin resistance can alter the function of the hypothalamus and the pituitary gland in the brain, thereby increasing the production of androgens. Additionally, elevated insulin level increases the secretion of luteinizing hormone which inturn promotes androgen production. Increased production of androgens in women will leads to hyperandrogenism.
Hyperinsulinaemia and hyperandrogenaemia changes the ovarian function and results in follicular arrest and anovulation (absence of ovulation). Studies showed that high androgen level is an independent risk factor for PCOS resulting in female infertility and ovarian dysfunction. [12,13]
Hypothyroidism in PCOS: Relation with Obesity
Obese women have slightly high levels of thyroid stimulating hormone (TSH) than normal weight individual. Excess body weight slows down the thyroid function and results in hypothyroidism (underactive thyroid), which have a negative impact on the ovaries. Several studies demonstrated that approximately 43% of women with PCOS suffer from subclinical hypothyroidism. [14]No simple cure for PCOS exists. But the symptoms can be managed to improve the fertility and decrease the risk of long-term complications. Engaging in regular exercise, keeping a healthy diet, losing excess weight, smoking cessation and taking the prescribed medications all plays an important role in the treatment of PCOS.
Lifestyle changes: Studies show that, weight loss of just 5% can lead to a significant improvement in PCOS symptoms. Changes in the quantity, type, and quality of dietary products, also change in the degree and type of physical activity have significant role in reducing body weight. Fibre-rich and low carbohydrate foods, such as whole-grain breads, cereals, whole-wheat pasta, brown rice, barley and beans can be included in the diet. Routine exercise for at least 30 minutes may have significant influence in obesity among PCOS women.
Medications: Certain medicines are prescribed to regulate menstrual cycle, reduce excessive hair growth and promote normal ovulation. Additionally, if diet and exercise doesn’t reduce weight certain weight-loss medications are prescribed.

Sleep apnea refers to a condition in which
58,936 total views, 59 views today

Since the beginning of 20th century, the overall
58,913 total views, 59 views today

New year is the time for new beginnings.
59,613 total views, 59 views today

Weight loss can be tricky business, as it
59,484 total views, 59 views today

According to a recent study, weight loss through
60,383 total views, 59 views today

According to a recent study, preoperative very low
60,384 total views, 59 views today
A recent study conducted on GERD (Gastroesophageal Reflux
60,388 total views, 59 views today
A recent study done to examine the long-term
59,270 total views, 59 views today

Overweight and obesity is a major health concern
29,555 total views, 43 views today

A recent study published in the Journal of
28,745 total views, 43 views today
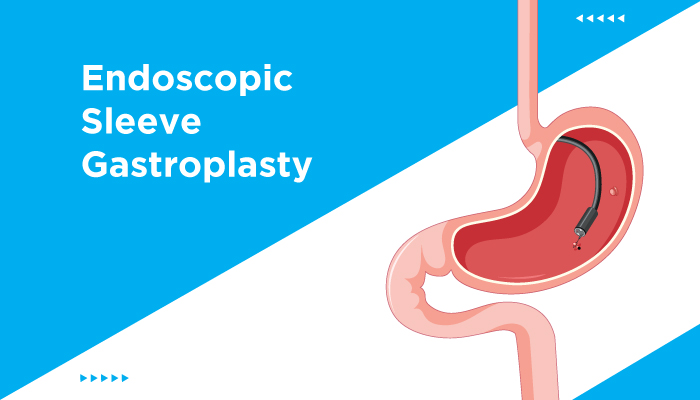
The findings from a recent study, published in
28,986 total views, 43 views today

The findings of a recent study, published in
29,386 total views, 43 views today

Sleep apnea refers to a condition in which breathing
58,937 total views, 60 views today

Since the beginning of 20th century, the overall obesity
58,914 total views, 60 views today

New year is the time for new beginnings. Most
59,614 total views, 60 views today

Weight loss can be tricky business, as it requires
59,485 total views, 60 views today

According to a recent study, weight loss through lifestyle
60,384 total views, 60 views today

According to a recent study, preoperative very low energy
60,385 total views, 60 views today
A recent study conducted on GERD (Gastroesophageal Reflux Disease)
60,389 total views, 60 views today
A recent study done to examine the long-term outcomes
59,271 total views, 60 views today

Overweight and obesity is a major health concern these
29,556 total views, 44 views today

A recent study published in the Journal of Clinical
28,746 total views, 44 views today
The findings from a recent study, published in the
28,987 total views, 44 views today

The findings of a recent study, published in Lancet,
29,387 total views, 44 views today

Dietary modifications, along with regular exercise, play an important
11,932 total views, 14 views today

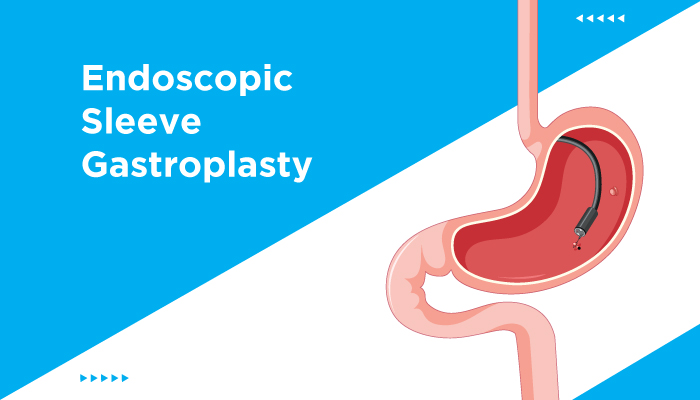
The findings of a recent study, published in the
5,752 total views, 2 views today

A study published in Science Daily stated that a
5,848 total views, 2 views today